ARTICLES
My Experience with GDV
Just to add a little stress to my life (on top of moving, and changing careers), one of my kids - ok, fur-babies - decided she wanted to know what kind of dog treats they served in heaven. I am so fortunate to say that it wasn’t her time just yet.
Let me back up a little bit… About two and a half weeks ago, a horrible thing happened to my favorite berner, Raven. She developed a condition called gastric dilatation-volvulus (GDV, or more commonly known as “bloat”), where the stomach dilates and then rotates (think Marley and Me), cutting off entry and exit to the stomach as well as blood flow to important internal organs, causing a host of horrible problems. The cause of this condition is not completely understood by the veterinary community, but one thing is for sure - this is a life threatening emergency that requires an immediate response.
Sunday Late Night: My husband, Jake, rushed Raven to the emergency veterinary hospital Sunday night and I hurried to meet him there. The diagnosis was confirmed with a radiograph, though Raven displayed classic GVD clinical signs. Surgery or euthanasia were our only options; luckily we had caught it early, and with surgery the prognosis was decent. We opted for surgery.

Monday Early Morning: For several agonizing hours, we waited for a phone call from the doctor. The call eventually came, and he told us the surgery went well. The stomach was bruised, but we were told that the tissue looked viable. The doctor re-oriented the stomach, tacked the stomach to the abdomen wall (gastropexy) to prevent future rotations, and closed Raven up. She would have to stay a day or two in the hospital while she recovered. All in all, things were ok.
Monday: We received a phone call from the veterinarian managing Raven’s post op care. She said that Raven’s stomach began to dilate again around 9 a.m. The gastropexy stopped any rotation that might have happened but they still passed an orogastric tube to relieve the pressure. The doctor was not horribly concerned about the incident and suggested that some post GVD ileus might be to blame. Raven was still set to come home on Tuesday. We stopped by in the evening to visit Raven. The technician brought us some canned food in a bowl to see if she would eat. She scarfed it down. At that moment the doctor came back in the room to chat with us. She was surprised and pleased that Raven had such a good appetite. I jokingly stated that if Raven ever stopped eating we would know she was an inch from death because she is the most food motivated animal I have ever met.
Tuesday Morning: We were informed that Raven developed a mild fever during the night. The overnight doctor mentioned that she had some trouble with her IV catheter which could be causing the fever. To be safe, they were going to take chest radiographs in a little bit to rule out aspiration pneumonia and get back to us with the results.
Tuesday Evening: Jake and I stopped by the hospital on our way home to see Raven. When we arrived, we were told that Raven had not wanted to eat all day. Her fever was higher despite not having pneumonia and being switched to a broader spectrum antibiotic. Her abdomen also seemed very painful and she seemed distressed. The doctor said that it could potentially be pancreatitis and that if she wasn’t doing better by the morning that they would schedule an ultrasound. Raven was obviously not ready to go home.
On the way home from our visit, I got a phone call from one of my good friends, who also happens to be a veterinarian. We had been keeping her and her husband updated with Raven’s status and I had just sent her a text message with the latest info. She was calling to tell us that we should transfer Raven to a speciality center for the remainder of her recovery, as a precaution, because the recovery was not progressing in a typical fashion (later she would tell me that she was concerned about Raven but did not want me to be worried). This other hospital was staffed with many amazing specialists (ER doctors, criticalists, internists, etc.) and they would be well equipped to handle problems should one come up. Jake and I agreed, and we turned around to pick Raven up and bring her straight to the other hospital.

Tuesday Late Night: We arrived at the new hospital and they immediately brought Raven to the back for an exam. A few minutes later, the ER doctor came in to talk with us - it was not good news. Raven had a lot of free fluid in her abdomen. They took a sample of it, along with some blood, and ran a few tests. Our doctor was very concerned that something had gone wrong. She informed us of our options, the most aggressive of which being going back in for an exploratory surgery that night. We opted to do the second surgery, gave Raven a few hugs, and headed home.
Wednesday Early Morning: We waited for another agonizing few hours. Before we left the hospital, the ER doctor had told us that there was a possibility that the surgeon might open Raven back up and find that there was nothing that could be done (there could be too much necrosed tissue, the stomach could have ruptured, etc.) and that the most humane thing to do might be to euthanize her on the operating table. If that was the case, they would call us immediately and it would likely be early on into the procedure. Every minute that ticked by was a blessing and curse - it meant that the surgeon was still working which was good, but that we didn’t yet know the outcome which drove me crazy.
When the call finally came, it was decent news. The surgeon told us a portion of her stomach had died but that the stomach had not ruptured. She was able to remove the dead tissue, and removed the spleen as well. She also placed a nasogastric feeding tube, a jejunostomy feeding tube, and a drain. There was a portion of stomach that she was concerned about but was not able to remove. However, there was still profusion of blood to that area so she was hopeful that the tissue would survive. The lining of Raven’s stomach had also turned black (indicating that it had died), and would slough off soon. All in all, she gave Raven a 50⁄50 shot of recovery.
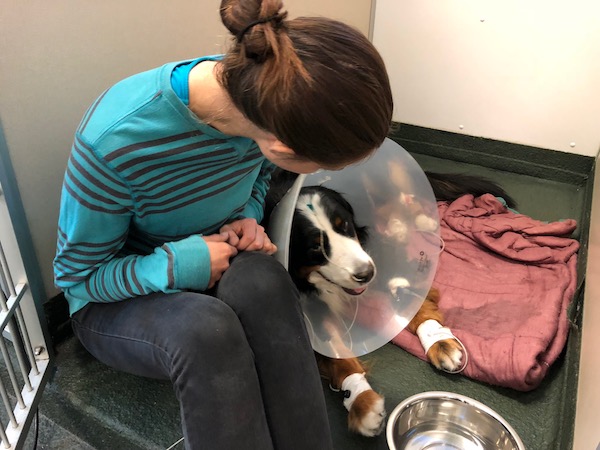
Wednesday Afternoon: Jake and I went to visit Raven at the hospital. She was resting comfortably in ICU. The hospital staff were monitoring her closely. We were feeling hopeful.
Thursday Morning: We received our morning update letting us know how Raven did overnight. Raven seemed a bit brighter and more active. She still was not interested in food but in general seemed to be doing better.
Thursday Evening: We drove back to the hospital to see Ray. We offered her food but she was not interested. She was, however, being fed through her nasogastric tube and her stomach was tolerating it which was a good sign.
Friday Morning: Our morning phone update was a bit unexpected. The internist told us that Raven had developed another low grade fever overnight. She also seemed less bright on exam. They were going to run a few more tests and get back to us.
Friday Early Afternoon: When the internist called back, I immediately knew from the tone of her voice that it was not good news. Her blood work showed a significant elevation in ALT (above 1000) and AST, her bilirubin was high, and her albumin was very low. She also appeared to be jaundiced on exam. Raven’s liver was failing. The internist said that it was possible that a clot had formed in her liver or her gallbladder. If there was a clot in the gallbladder, it might be possible to fix it surgically. I told her that we did not want to put Raven through another surgery. She understood and said that it was also possible that it could be an acute toxic insult to the liver due to all of the dead tissue the body was having to process. If this was the case, the good news was that Raven was already being treated in a way that they would treat liver toxicity - supportively on IV fluids. Her recommendation was that we give Raven 24-48 hours on supportive care and see if she shows signs of improvement.
Friday Evening: The technician brought us to a visiting room and went to get our fur-baby. Raven slowly walked into the room and slumped down on the floor, exhausted. Jake and I were heartbroken. Ray laid on the floor, giving us the smallest tail wag in between falling in and out of sleep. She was just a shadow of her formerly happy self. We sat with her for an hour, petting her and talking to her. Our doctor said that things weren’t looking great but that there was still some hope, and that we would probably have our answer by the end of the weekend. Raven deserved a little bit more time. She said that if it was liver toxicity, the beauty of the liver is that it is one of the organs that can regenerate itself, and it would be possible to recover.

Later that evening Jake and I met our friends (the husband and wife veterinary team that suggested we have Raven transferred) for dinner. They reassured us that giving Raven more time in the hospital was the best thing to do, is what they would do if it was their dog. We appreciated talking to them as friends and as doctors. We were very lucky to have them as a resource during this emotionally taxing time.
Saturday: Jake and I got our morning update phone call. Raven was able to rest that night and seemed just a tiny bit brighter that morning. She had some edema in her legs (likely because of her low albumin) and a mild fever. She was still weak but was no worse off than the day before. We went to visit her in the hospital, along with Jake’s parents. Raven was happy to see us and was a little more energetic. We were happy to see the tiny bit of improvement but did not want to get our hopes up just yet.
Sunday: Armed with a rotisserie chicken, my dad came to visit Raven with Jake and me. He was determined to tempt her to eat something. The doctor was pleased with our plan, as long as we only offered the white meat, and had the technician bring Raven to the visiting room. She walked in, still tired looking, but with more pep than the previous day. She still had a fever and some swelling, but was definitely overall a happier dog. She was making baby steps in the right direction. However, she still did not want to eat anything.
Monday: Our morning phone call was a welcomed one. Raven’s fever had broken overnight and she was alert and looking around. By the time we came to visit her, the doctors had taken her off of her fluids and removed the drain from her abdomen. A technician was able to coax her into eating a milk bone. We offered her some of the chicken my dad had brought yesterday and she ate a small piece. She was drinking water willingly in her kennel. The name of the game was baby-steps, and she seemed to be winning!
Tuesday: Raven continued to make small improvements throughout the day. The edema was decreasing and she ate a few more bites of milk bone. The doctor decided to run more blood work on her to see where things were at. Her ALT decreased a little, along with her bilirubin and AST. Her total protein and albumin were increasing, and she was less anemic. The criticalist told us that we were not out of the woods yet but the blood work results were encouraging.
Wednesday: I was waiting for my husband outside of his office (we were going to carpool to the hospital to see Raven) when he sent me a dog emoji via text message. My spousal mind reading super power kicked in. This could only mean one thing- Raven was coming home today! Jake got to the car and said he just took a call from the veterinarian. Raven was indeed well enough to come home.

We arrived at the hospital and a technician brought Raven into the room with us. I think she knew she was going home because she was a little more eager to leave the exam room. The technician went over our discharge instructions and we were out the door! When we got home, our other dog Maya greeted us at the door with a big tail wag and slightly nervous sniff. We walked Raven over to her bed where she happily laid down, excited to be home but still exhausted.
A bit later, per veterinary instruction, we tried offering a bunch of different foods to stimulate Raven’s appetite. Through some trial and error, we discovered that she disliked dog food in all forms (wet and dry) but cat food, eggs, turkey lunch meat, and dog cookies were ok. To my surprise and amusement, baby food completely disgusted her.
Thursday: Raven continued to eat small bits of certain foods (eggs were a favorite today) and rested a lot.
Friday: I had a follow-up appointment scheduled with the internist in the afternoon. That morning, I took Raven to my general practice clinic to run some more blood work before hand. This showed that her ALT was still very high (over 1000), but her albumin, bilirubin, AST, and total protein numbers were all moving in the right direction. The internist was not surprised that her ALT was still elevated but was encouraged that all of the other values were improving. That indicated that her liver was doing something. We weren’t out of the woods yet but we were still taking steps in the right direction, especially because clinically Raven appeared to be improving.
Saturday - Wednesday: Raven’s appetite and attitude continued to improve each day. On Tuesday, she decided to finally eat a little bit of kibble. She was more energetic and I could see bits of her personality shine through. Jake and I were finally feeling more positive about her prognosis. (Well, I should just say “I” was finally more positive. Jake always thought she was going to be ok, and I was a worry wart.)
Thursday: Raven had another follow-up appointment scheduled with the internist. This time, her blood work showed some very positive improvements. Her ALT was 320! This is still way above the normal range of under 140, but along with continued improvements in her other liver values, it was very good news. The internist confidently said that Raven’s most recent blood work was a “positive prognostic indicator”, which translated to regular speak, means she is likely (finally) in the clear! We were instructed to recheck blood work in two to three weeks and send her the lab results. I crossed my fingers that we would see continued improvement each day!
Thursday Afternoon: And here I am, writing this blog post, with my baby Ray sitting next to me on the couch. She is almost herself, and her once annoying habit of gazing longingly at my food with her head in my lap is now the most welcomed sight. Her appetite is back, she wants to eat my food, and I am gratefully willing to give her a little bite. Thanks to the work of some amazing doctors and technicians, and to the speedy actions of my husband in getting her to the hospital, Raven is going to live to see Alaska. She is going to be ok.
